Alcoholism Cirrhosis: Signs, Symptoms, Risks
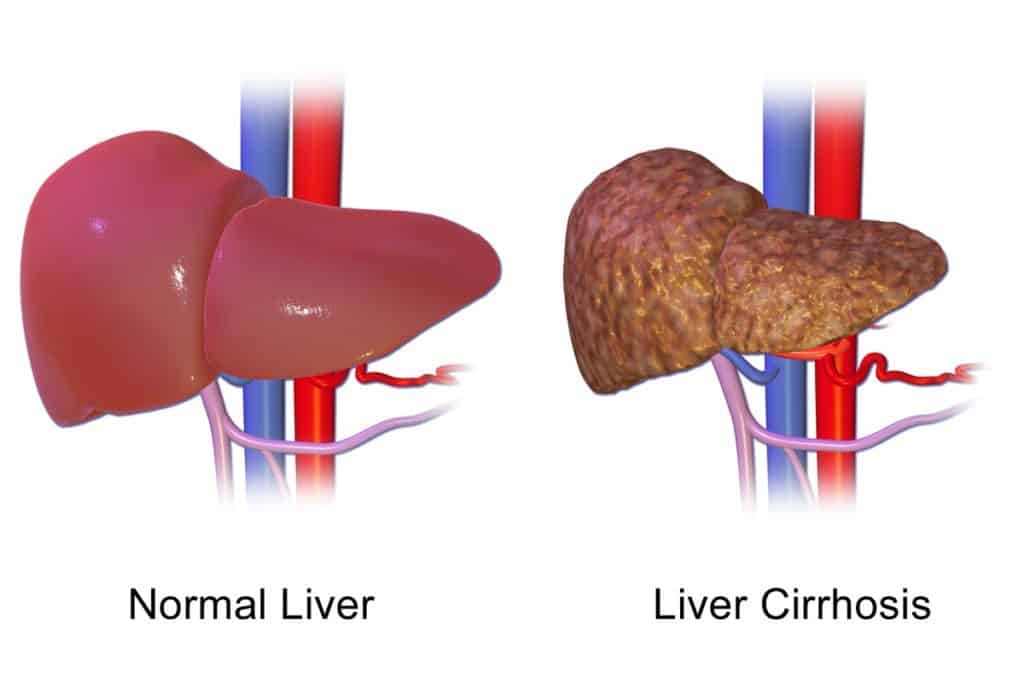
Cirrhosis is the advanced scarring of the liver caused by long-term liver diseases. This scarring can happen because of hepatitis, fatty liver disease, and chronic alcoholism, according to the Mayo Clinic.(1)
Someone who continues drinking with cirrhosis isn’t allowing their liver to repair itself. This results in scar tissue forming, thus making it difficult for the liver to function. In some cases, advanced cirrhosis can threaten your life or even be fatal.
Some people may not realize they have cirrhosis from alcoholism or recognize its symptoms. The condition works slowly, but if not dealt with, can lead to complications that stick with you for the rest of your life. So how can you halt the effects of alcoholism cirrhosis and what are alcoholism cirrhosis symptoms?

Alcoholism Cirrhosis
Alcoholism-related cirrhosis is, unfortunately, a common disease. Healthline and the American Liver Foundation report that 10–12% of heavy drinkers in the U.S. will develop it(2).
Drinking too much alcohol is the leading cause of alcohol-related cirrhosis. When you consume more alcohol than your liver can handle, it becomes damaged. As your liver breaks down alcohol, it produces a toxin that harms liver cells.
Heavy alcohol consumption over a long time will repeatedly damage the liver and affect your whole body. Other factors can mix in with drinking to develop alcoholism cirrhosis. Carrying extra weight, eating poorly, and having a family history of hepatitis can raise your risk of developing cirrhosis.
Check Your Insurance Coverage for FREE
Find out if your insurance covers addiction treatment in minutes. We accept most insurance!
Risk Factors That Contribute to Alcohol-Related Liver Damage
Several risk factors can increase the chances of developing cirrhosis from alcohol use. The most significant factor is the amount of alcohol consumed over time. People with alcohol use disorders often underestimate how much they drink. The liver can only process a certain amount before it becomes overwhelmed.
When alcohol intake consistently exceeds this limit, the liver produces toxins that begin damaging liver tissue. Over the long term, this damage leads to scarring and loss of function.
Individuals with an alcohol addiction who drink daily or binge drink face the highest risk. However, cirrhosis can still develop in individuals who drink moderately but do so over many years. Other risk factors include co-occurring conditions such as hepatitis B or C, which accelerate liver decline. People with alcohol use disorders who contract viral hepatitis often experience faster and more severe liver damage.
Nutrition also plays a critical role. Individuals who abuse alcohol frequently lack proper nutrients that help maintain liver health. Deficiencies in vitamins like A, D, and E leave liver tissue more susceptible to inflammation and scarring.
Being overweight or having metabolic syndrome further increases the strain on the liver. It makes it harder for the organ to repair itself.
Social and psychological influences can also shape alcohol intake. People with alcohol dependency who experience stress, mental health issues, or lack support are more likely to drink heavily. Over time, this creates a cycle of damage that becomes harder to reverse.
Recognizing these risk factors early allows people to make informed decisions about their health. Reducing alcohol intake, seeking medical guidance, and making lifestyle changes can prevent the progression of liver damage.
Alcoholism Cirrhosis Symptoms & Stages
A drinker goes through several stages before reaching alcoholic liver cirrhosis. It can start with fatty liver disease. This is when fat builds up inside liver cells, making it harder for the liver to do its everyday functions. Usually this stage is symptom free, besides the possible pain on the right side of the stomach from an enlarged liver.
Fatty liver disease can turn into alcoholic hepatitis. Alcoholic hepatitis is the killing of liver cells, along with inflammation. This when we fibrosis develops. Fibrosis is scarring of the liver.
Eventually these two stages lead to alcoholism cirrhosis. In some cases, people have skipped the earlier stages and developed alcoholic liver cirrhosis.
Symptoms of the condition generally begin in drinkers between the ages of 30 and 40. At first, a body is able to make up for your liver’s difficulty working. But as the cirrhosis develops, symptoms are more apparent. Some alcoholism cirrhosis symptoms are:
- Jaundice, the yellowing of the skin and whites of the eyes.
- Portal Hypertension, which is the rising of the pressure in a portal vein. The portal vein carries blood from organs to the liver.
Itching of the skin. - Itching of the skin
According to the NHS, some other alcoholism cirrhosis symptoms are abdominal pain, loss of appetite, fatigue, and diarrhea(3). Advanced alcoholism cirrhosis symptoms often present more visibly.
NHS states these complications of cirrhosis as:
- Swelling in the legs ankles and feet caused by a build-up of fluid (oedema)
- Swelling in your abdomen caused by a build-up of fluid known as ascites
- A high temperature and shivering attacks
- Hair loss
- Curved fingertips and nails
- Blotchy red palms
- Significant weight loss
- Muscle wasting
- Confusion and memory problems
- Trouble sleeping
- Changes in your personality (caused by a build-up of toxins in the brain)
- Passing black, tarry poo and
- vomiting blood as a result of internal bleeding,
- a tendency to bleed and bruise more easily,
- increased sensitivity to alcohol and drugs and because the liver cannot process them.
In extreme cases, cirrhosis can lead to liver cancer.
Drinking with Cirrhosis and Alcoholism Cirrhosis Treatment
Once someone has fatty liver, alcoholic hepatitis, or cirrhosis, the best thing to do is stop drinking right away. They should remain abstinent from alcohol even after their health begins to improve. According to Medical News Today, quitting alcohol after a diagnosis of fatty liver disease may reverse the condition. This reversal can occur within 2 to 6 weeks (5).
For people with cirrhosis, any health improvements from not drinking usually disappear if they start drinking again. Chronic drinkers should not stop drinking without medical support, as it can be life threatening.
Chronic drinkers seeking to quit should seek medical support from a hospital, detox, or rehab. Medications such as benzodiazepines can ease alcohol withdrawals in someone with an alcohol addiction.
Once you have achieved some physical sobriety and your health has improved, you can maintain a life without alcohol. You can achieve this through 12-step programs like Alcoholics Anonymous. Therapy can help address root psychological trauma and emotional triggers of drinking. Additionally, medications such as acamprosate, naltrexone, topiramate, baclofen, and disulfiram can help reduce relapses.
For individuals who continue drinking despite having cirrhosis and ignore the warning signs, liver failure is inevitable. At that point, survival depends on receiving a liver transplant. A liver transplant is not guaranteed, as hospitals have strict criteria and do not offer transplants to everyone.
A person must be sober for six months and show major improvements in their health before doctors will consider them for a transplant. The procedure is complex and can only happen if a donor is available. Even if the surgery goes well, problems can still happen afterward, and recovery is not always easy.
People can live a normal life after recovering from alcohol cirrhosis. The key is to catch alcoholism cirrhosis early. When someone shows signs of alcoholic cirrhosis, they need to stop drinking and potentially enter a medical detox program. Their survival depends on giving their liver a chance to heal.
Reach out to Hotel California by the Sea
We specialize in treating addiction and other co-occurring disorders, such as PTSD. Our Admissions specialists are available to walk you through the best options for treating your addiction.
References:
- Cirrhosis – Symptoms and causes – Mayo Clinic
- Alcoholic Liver Cirrhosis: Causes, Symptoms & Diagnosis (healthline.com)
- Alcohol-related liver disease – Symptoms – NHS (www.nhs.uk)
- Alcohol-related liver disease – Symptoms – NHS (www.nhs.uk)
- Alcoholic liver disease: Symptoms, treatment, and causes (medicalnewstoday.com)