Integrating Behavioral Health and Primary Care
There has been an increasing uptick in mental health conditions over the past few years following the Covid-19 pandemic. Because of these rising figures, advocates are calling for mental health care to be integrated into general health care practices. Millions of people in the U.S. have physical, mental health or substance use illnesses. Some even have a combination of two or three conditions. Unfortunately, treatment for each of these conditions falls under separate healthcare entities. This makes it much more challenging to navigate multiple healthcare systems. It also makes it more difficult to accurately diagnose and treat physical and mental disorders.
Physical and behavioral health care systems operate separately without coordination. This leads to gaps in care, inappropriate treatments as well as increased healthcare costs. It could ultimately result in a worse outcome for those who live with both physical and behavioral conditions.

By integrating behavioral health and primary care, there is a greater potential to help those who are suffering from mental illness or substance abuse conditions. This helps to normalize and de-stigmatize mental health and behavioral health disorders. Integrating mental health into primary care also helps to ensure that an overall health assessment can be addressed holistically. Ultimately leading to better treatment options and greater quality of life for all patients. All people with mental health and substance health conditions deserve accessible, affordable and comprehensive health care.
What is Behavioral Health?
Behavioral health care consists of the prevention and treatment of mental health conditions, substance use disorders and overall emotional well-being. Behavioral health care supports those who are experiencing or recovering from any of these conditions. This type of health care system has traditionally and historically been separate from other avenues of health care.
Despite the clear separation, physical health and behavioral health are closely linked. The actions and symptoms of a physical condition can greatly impact a person’s mental and emotional situation. The same can be said of a psychological condition contributing to the development of physical health issues.
Behavioral health is among the most undertreated medical conditions where only one-third of people with symptoms actually receive the care they need. Today the U.S. is experiencing a behavioral health crisis. The number of people experiencing mental health conditions and substance use disorders is increasing despite the limited access and options for necessary treatment. Two of the significant contributions of the behavioral health crisis are the shortage of behavioral health providers and limited insurance coverage options for treatment services.
Advocates for integrated health solutions believe incorporating mental and emotional health services into general public health prevention and treatments can significantly promote a more effective health care system. Like any other physical illnesses and ailments, prevention, early detection and treatment of behavioral conditions can lead to improved overall community health.
Integrating Behavioral Health and Primary Care
In an effort to bring together behavioral and physical health care services, the introduction of integrative health solutions can help produce better health outcomes for all. Integrative mental and physical health services provide a holistic view of a person’s health. It addresses physical, emotional, and psychological aspects of health and how each affects each other. Integrated health solutions can improve access to care, improve coordination of care and improve quality of care.
Oftentimes, people hesitate to seek treatment from their primary care providers for any mental health conditions. Primary checkups mainly consist of addressing physical ailments. Concerns over mental and emotional health are occasionally addressed but only if the patient brings them up. Due to stigma and stereotypes, many people are less likely to receive the help they need unless treatment is integrated into routine primary care wellness assessments. In some cases, patients are unaware or unsure of the conditions they have and what treatments they may need. The disconnect in types of treatment only worsens the issues and can delay diagnosis and treatment.
In a better effort to bring awareness to integrative behavioral and physical health care, the Mental Health Parity and Addiction Equity Act (MHPAEA) was created. The MHPAEA requires all healthcare providers to offer behavioral health benefits that are considered on par with medical benefits. It is a federal law that prevents medical groups and insurance that provide mental health treatment and substance use disorder services, from imposing fewer benefit options and limitations on behavioral health coverage and care.
Check Your Insurance Coverage for FREE
Find out if your insurance covers addiction treatment in minutes. We accept most insurance!
Benefits of Integrating Mental Health into Primary Care
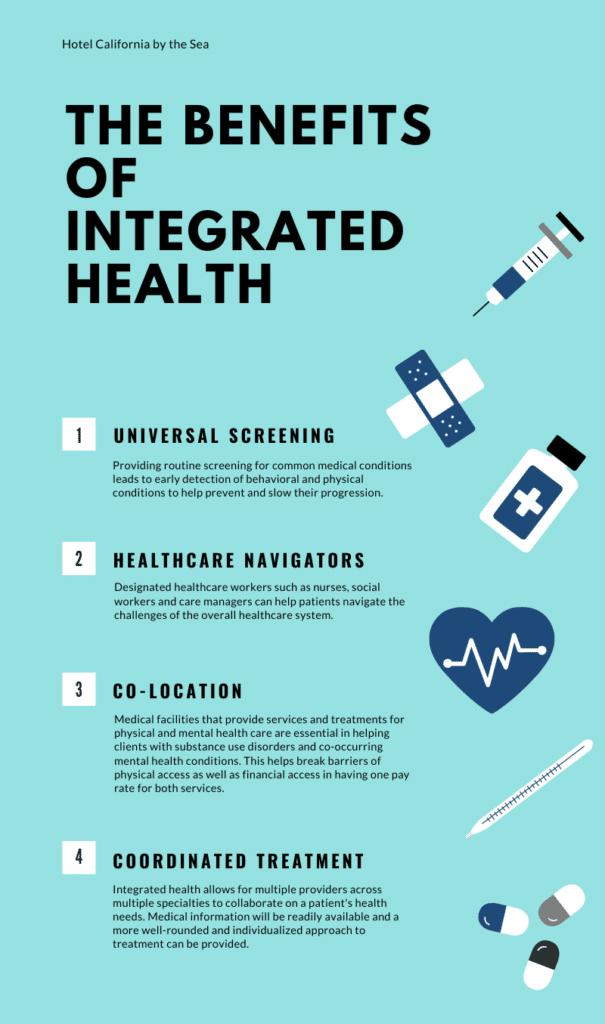
- Universal screening: Provide routine screening for common medical (behavioral and physical) conditions. Early identification of any conditions can help prevent and slow their progression.
- Navigators: Healthcare workers such as nurses and social workers can be designated to help patients navigate the challenges of insurance and the overall healthcare system. They will help clients find care, interact with their healthcare providers on their behalf and help implement and improve home and community support.
- Co-location: Onsite facilities and services that readily and easily provide treatment for both physical and mental health are crucial. Not only should services be in the same physical area, but creating a single pay rate for both services can also be a huge benefit.
- Coordinated treatment: Integrated health services allow multiple types of providers who collaborate to address all of a patient’s health needs. This also allows for shared medical information between all of the patient’s providers. Access to a full health assessment can help better coordinate appropriate individualized care for the patient.
Reach out to Hotel California by the Sea
We specialize in treating addiction and other co-occurring disorders, such as PTSD. Our Admissions specialists are available to walk you through the best options for treating your addiction.
Hotel California by the Sea is a behavioral health care provider helping people with substance use disorders and co-occurring mental health conditions. Substance abuse and mental health often develop concurrently having impactful effects on each other. Therefore, in order to create a successful recovery outcome, the two conditions should be treated together.
The dual diagnosis program focuses on helping people overcome their addictions through evidence-based treatments and a wide range of care programs. Various levels of care include detox, residential treatment, PHP and IOP programs. Rigorous treatment methods include CBT, EMDR therapy and family therapy allowing patients to learn effective coping techniques to help them navigate sober living. Hotel California by the Sea believes in helping clients overcome their addictions through individualized treatment plans addressing the unique obstacles of each client’s recovery.
References:
https://www.nami.org/Advocacy/Policy-Priorities/Improving-Health/Physical-Mental-Health-Integration
https://www.samhsa.gov/sites/default/files/samhsa-behavioral-health-integration.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5854169/
https://www.healthleadersmedia.com/payer/why-its-time-integrate-behavioral-and-physical-health